Medical Interventions: Risks, Benefits & Alternatives
- AH Apothecary

- Apr 8, 2024
- 5 min read

It can be very overwhelming navigating the medical world when you first find yourself pregnant and in the care of strangers. It is important to be able to give informed consent to any and all potential procedures thrown at you from your first appointment to your very last.
So what is informed consent? Informed consent is defined as "the willing acceptance of a medical intervention by a patient after adequate disclosure by the physician of the nature of the intervention with its risks, benefits and alternatives."
Informed consent is NOT the same as signing a consent form. A consent form only documents the process and the patient's decision. A consent form does not have legal authority over a patient and is not legally binding. A patient cannot sign away their civil rights. Consent forms are created to protect the hospital and care providers. They do not have the power to limit the right of the patient.
Informed consent is owed every step of the way and may be altered at anytime by the patient via written or spoken word. a simple "No" or " I do not give consent" is enough. "No" is a complete sentence that a women does not have to justify. Being admitted into a hospital does NOT imply consent nor does signing a consent form. Often times, routine procedures are presented as non-optional and no information is given on the risks. Many care providers are unaware of their involvement in violating a patient's rights and are just doing as they are told/trained. When a procedure or intervention is brought up without the discussion of risks and patients aren't given a choice, it is a deep violation of their human rights.
You have the right to informed consent and refusal of any medical intervention and being pregnant does not remove this right. As said by ACOG, "The freedom to accept or refuse recommended medical treatment has legal as well as ethical foundations. In the obstetrics setting, recognize that a competent pregnant woman is the appropriate decision maker for the fetus that she is carrying."
Here's an overview of common interventions and procedures during pregnancy, birth, and postpartum care, along with their associated risks, benefits, and alternatives:
Induction of Labor:
Risks: Increased risk of cesarean birth, fetal distress, uterine rupture, and postpartum hemorrhage. Increased discomfort due to the intensity of artificially induced contractions.
Benefits: May prevent complications associated with prolonged pregnancy and reduce the risk of stillbirth in certain high-risk situations such as poor fetal growth or intrauterine growth restriction (IUGR), premature rupture of membranes, maternal infection of the fetal membranes (chorioamnionitis), gestational diabetes, preeclampsia, or chronic hypertension that could compromise maternal or fetal health.
Alternatives: Waiting for spontaneous labor, membrane sweeping, natural methods to encourage labor (such as walking and nipple stimulation), vaginal steaming (after 37 wks), activities that increase oxytocin (hugging, eye contact, singing, dancing, laughing, orgasming, nature walks, bubble baths). Continuous Fetal Monitoring:
Risks: Increased risk of unnecessary interventions, such as cesarean birth, due to false alarms.
Benefits: Early detection of fetal distress, which can guide timely interventions to prevent complications.
Alternatives: Intermittent fetal monitoring, especially in low-risk pregnancies, use of dopplers.
Epidural Anesthesia:
Risks: Potential for decreased mobility during labor, which can prolong labor and increase the likelihood of instrumental delivery.
Benefits: Effective pain relief during labor, which can improve maternal satisfaction and reduce the risk of trauma associated with unmanaged pain.
Alternatives: Non-pharmacological pain relief methods (e.g., massage, hydrotherapy, breathing techniques, doulas), systemic opioids, or regional anesthesia techniques like combined spinal-epidural. Cesarean Birth:
Risks: Increased risk of infection, blood loss, and longer recovery time compared to vaginal birth, bypassing vaginal microbiome.
Benefits: Necessary in certain situations to protect the health and safety of the mother and/or baby, such as fetal distress or placenta previa.
Alternatives: Vaginal birth after cesarean (VBAC) for eligible candidates, assisted vaginal delivery (forceps or vacuum extraction) if appropriate. Episiotomy:
Risks: Increased risk of perineal trauma, severe tearing (3rd & 4th degree tears) pain, and extended healing time compared to natural tearing.
Benefits: Controlled incision may prevent severe tearing and reduce the risk of pelvic floor dysfunction, may help expand space for shoulder dystocia if birthing on your back.
Alternatives: Allowing for spontaneous tearing, perineal massage during labor to promote tissue elasticity, warm compress by provider, birth/push in an upright position (squatting, all-fours, standing). Delayed Cord Clamping:
Risks: Slight increase in the risk of jaundice requiring phototherapy.
Benefits: Improves neonatal outcomes by increasing iron stores, reducing the risk of anemia, and enhancing cardiovascular stability and respiratory system.
Alternatives: Early cord clamping, especially in situations where immediate resuscitation of the newborn is necessary. Postpartum Pitocin (Oxytocin) Administration:
Risks: Increased risk of uterine atony, which can lead to postpartum hemorrhage.
Benefits: Reduces the risk of postpartum hemorrhage by promoting uterine contractions and reducing blood loss.
Alternatives: Physiologic management of the third stage of labor (e.g., delayed cord clamping, breastfeeding initiation, fundal massage). Glucose Tests (Gestational Diabetes Screening):
Risks: Discomfort from blood draw, false positives leading to unnecessary anxiety and interventions.
Benefits: Early detection and management of gestational diabetes, which reduces the risk of complications for both mother and baby.
Alternatives: Continuous glucose monitoring, dietary modifications, and regular physical activity to manage blood sugar levels, The fresh test, linked here. Frequent Ultrasounds:
Risks: Theoretical risk of potential harm to the fetus due to ultrasound exposure, increased medicalization of pregnancy leading to unnecessary interventions.
Benefits: Provides valuable information about fetal growth, development, and well-being, helps detect potential complications early.
Alternatives: Limited ultrasound scans based on medical necessity, such as anatomy scan, growth scans, and Doppler studies. Group B Streptococcus (GBS) Testing:
Risks: False-negative results leading to inadequate treatment, overuse of antibiotics contributing to antibiotic resistance.
Benefits: Identifies pregnant women carrying GBS, allowing for timely administration of antibiotics during labor to reduce the risk of neonatal infection.
Alternatives: Intrapartum risk-based screening for GBS colonization in the absence of universal testing, increase consumption of fermented foods (kefir, kombucha, sauerkraut,) and antibacterial herbs such as oregano oil in a carrier oil like coconut oil and then retesting. Laboring on Back (Supine Position):
Risks: Decreased blood flow to the uterus and fetus, increased risk of fetal distress and prolonged labor.
Benefits: Provides easier access for healthcare providers, facilitates monitoring and interventions during labor.
Alternatives: Upright positions (e.g., standing, walking, squatting, hands and knees) that may promote more efficient contractions, reduce pain, and improve maternal comfort and fetal well-being. Cervical Exams:
Risks: Risk of infection, discomfort, increased anxiety, and psychological distress.
Benefits: Provides information for provider about cervical dilation, effacement, and fetal position, which can help assess progress in labor.
Alternatives: Limiting unnecessary cervical exams, using other clinical indicators of labor progress (e.g., maternal behavior, contractions pattern, the purple line test and fetal descent). Baby Aspirin for Hypertension (Preeclampsia Prevention):
Risks: Potential side effects such as gastrointestinal upset and bleeding disorders.
Benefits: Reduces the risk of developing preeclampsia and its complications, including preterm birth and fetal growth restriction.
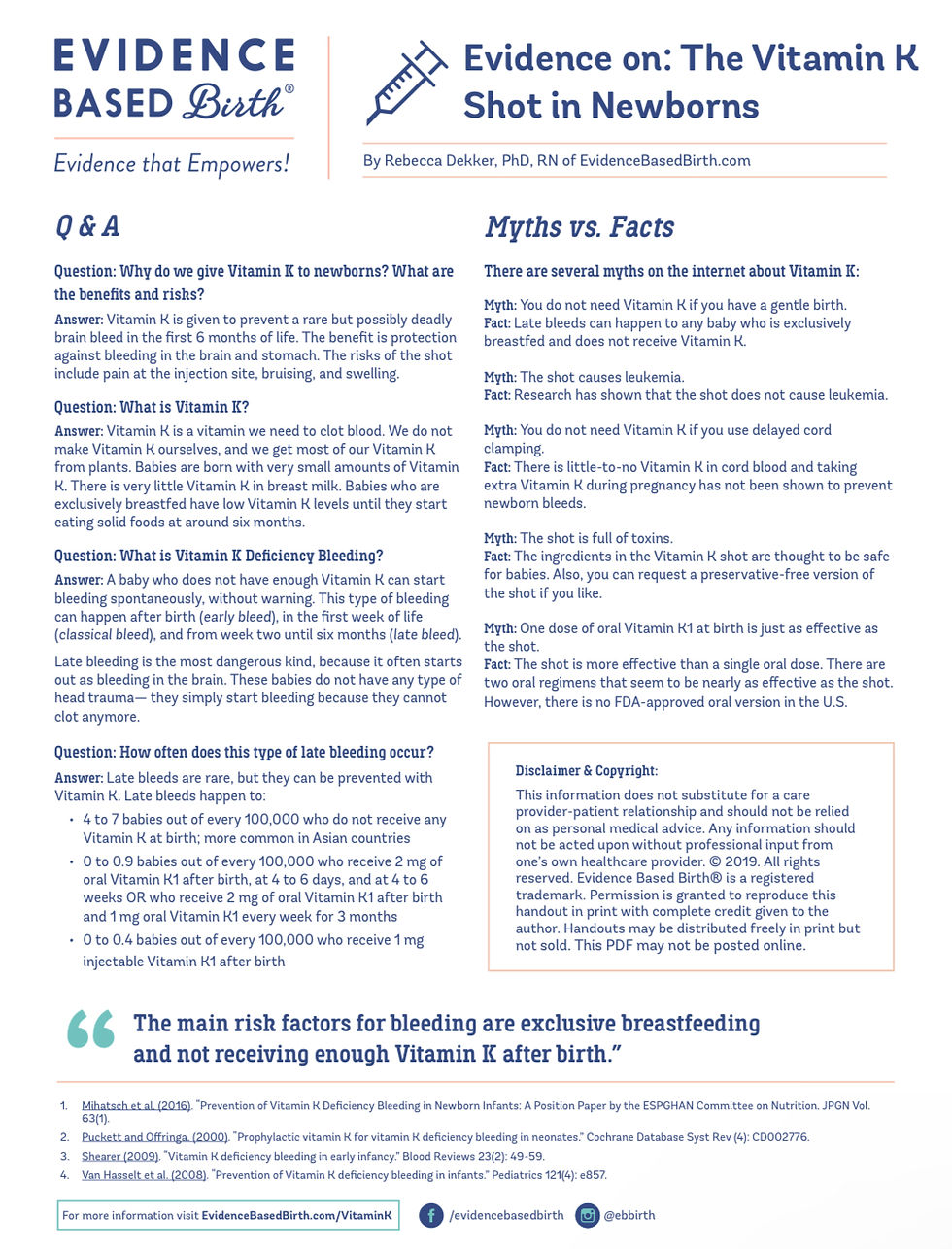
Alternatives: Lifestyle modifications (e.g., diet, exercise), grounding & breath work, calcium supplementation, cayenne pepper in a shot glass of water daily, and close monitoring of blood pressure. Vitamin K Shot for Newborns:
Risks: Potential risk of injection site reactions, rare allergic reactions.
Benefits: Prevents Vitamin K deficiency bleeding (VKDB) in newborns, which can cause severe bleeding and even death.
Alternatives: Oral Vitamin K supplementation, though it may be less effective than the shot in preventing VKDB, "preservative-free" vitamin k injections.
Erythromycin Eye Ointment (Ophthalmia Neonatorum Prophylaxis):
Risks: Potential for eye irritation and transient blurred vision which can affect proper bonding during the golden hour after birth.
Benefits: Prevents neonatal conjunctivitis caused by certain bacteria, including those responsible for sexually transmitted infections like chlamydia and gonorrhea.
Alternatives: Screening and treatment of maternal infections can reduce the risk of transmission to the newborn and applying breastmilk via an eye dropper.
As with any medical intervention, it's essential for pregnant individuals to discuss these options with their healthcare providers, considering individual circumstances, preferences, and the most current evidence-based information available.









Comments